 This is a guest post by Dehunge Shiaka, a gender expert in Sierra Leone. This is post #3 of a series he has written on the impacts of Ebola in Sierra Leone (post 1, post 2).
This is a guest post by Dehunge Shiaka, a gender expert in Sierra Leone. This is post #3 of a series he has written on the impacts of Ebola in Sierra Leone (post 1, post 2).
How can we ensure that when Ebola ends, Sierra Leone’s medical infrastructure and economy doesn’t disintegrate with it? Yesterday Oxfam called for an Ebola Marshall Plan to help countries like Sierra Leone, which have been seriously impacted by the deadly virus. This would involve economic interventions in health, education, and sanitation- amongst other areas. But given the slow and late response to the Ebola crisis- is this realistic?
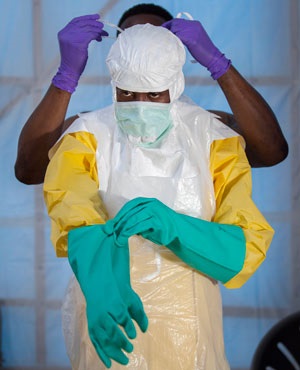
With criticisms levied against the world community for responding rather too late to the Ebola outbreak in Sierra Leone, various countries and international organizations and agencies including the AU, ECOWAS, UNMEER, WHO, WFP, UNICEF, WHH , CDC, MSF, Goal and Save the Children have recently stepped up their efforts to help the government contain the epidemic. More money and logistic supplies including ambulances, drugs and medical equipment worth millions of US dollars have been donated by the international community. More doctors, nurses and others have arrived from other countries such as Nigeria, South Africa, UK, US, China, Cuba, Canada, Spain, Italy, Australia and Ireland to serve as frontline health workers.
Any effective notion of an Ebola Marshall plan should be in the form of a partnership rather than a Western-led plan. What now remains is for government authorities to effectively link existing efforts with local actors and follow-up on service delivery in a coordinated way. The aim should be to stop Ebola in its tracks, and in the process strengthen the health system which appears to be on the verge of collapse.
Here’s what that might look like: Of course the British Army has set up Command Centres in all twelve districts in the western area, which are designed to reduce delays and improve ways of dealing with surveillance alerts, live cases, laboratory tests, quarantine and burial managements. There is a significant improvement in service response, as a result. Two months ago, the toll-free 117 Ebola hotline had only 12 operators and 18 lines which created a great deal of frustration among people who called and waited forever. Today, the hotline not only endeavors to answer all calls, but would call back to check whether the ambulance service has arrived. This is because 117 now has 60 operators and 90 lines. Similarly, holding and treatment centres have increased from 10 two months ago, to 16 currently with four more becoming operational by the end of 2014, which should be able to meet an expected 1,000 beds.
Such coordination mechanism should be strengthened among existing Ebola response structures and pillars, rather than allow competition among them. It is therefore important that critical support is channeled to the Ministry of Health and Sanitation for additional staff and capacity training and logistics so that it carries out its oversight role in case referrals and management, as well as in the distribution of drugs and other medical equipment to the various treatment centres. In this regard, the Ministry should be able to follow-up on rapid patient referrals from communities to isolation centres and on to treatment centres. It should also be able to put in place structures to follow-up on the work of surveillance officers, contact tracers and health education personnel in the field.
With a well-coordinated response structure in place available services and gaps are mapped out and fed into reporting system, personnel data set up to avoid delays in payments, and individual and community action monitored for impact. All these measures could contribute to ensuring that Ebola fizzles out in next few weeks, but also that the health system doesn’t fizzle with it.
Megan MacKenzie is a Senior Lecturer in the Department of Government and International Relations at the University of Sydney in Australia. Her main research interests include feminist international relations, gender and the military, the combat exclusion for women, the aftermaths of war and post-conflict resolution, and transitional justice. Her book Beyond the Band of Brothers: the US Military and the Myth that Women Can't Fight comes out with Cambridge University Press in July 2015.
https://www.cambridge.org/ee/academic/subjects/politics-international-relations/international-relations-and-international-organisations/beyond-band-brothers-us-military-and-myth-women-cant-fight?format=PB

0 Comments