This is a guest post from Heeun Kim, a PhD Candidate in the Department of Public Administration at Rockefeller College of Public Affairs and Policy, University at Albany. Her research focusses on access to healthcare, disparities in health, and universal health coverage. Her current research projects include sexually transmitted diseases prevention in New York State, disparities in access to care under the Affordable Care Act in the US.
As the US struggles to ramp up its COVID-19 response amid what appears to be widespread community transmission, countries that appear to have turned the corner on new infections can offer lessons.
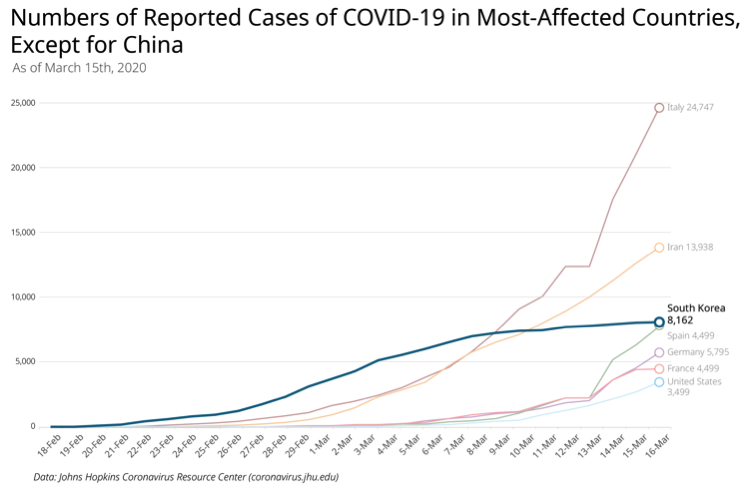
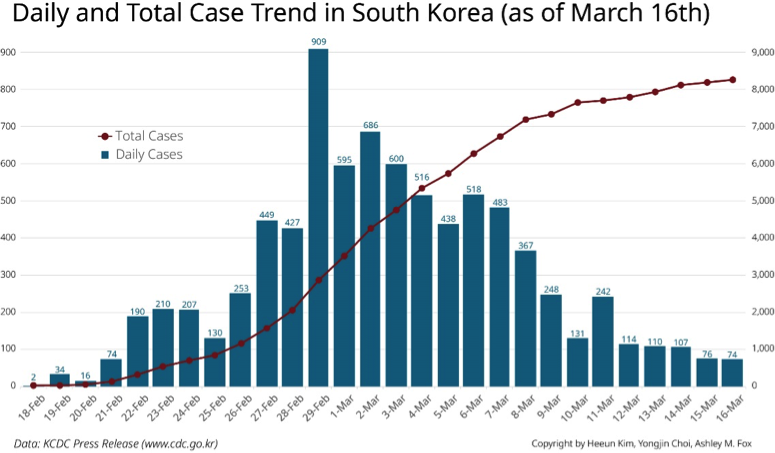
South Korea has been battling COVID-19 since the number of confirmed cases began skyrocketing in late February reaching nearly 8,000 confirmed cases with 67 patients deceased as of March 13. While Korea had, up until recently, the second largest number of confirmed cases after China, the number of newly confirmed cases has been declining for the last few days in the epicenter of the city of Daegu and adjacent regions (however, the number of community-level cluster transmissions has been gradually increasing in other cities). Moreover, its recorded case fatality rate is closer to 0.87%, rather than the 2-3% range reported elsewhere, which is likely to be more accurate than in other countries, due to widespread testing, but also possibly reflecting a more effective response or other underlying factors.
Notably, South Korea appears to have brought the outbreak under control in spite of an initially tepid political response, by adopting strategies that maximized transparency and access to testing, while managing to avoid draconian measures such as strong forms of social distancing and quarantine. It might be too early for an optimistic forecast, but these are some lessons from the South Korean case.
Key takeaways from South Korean Case
- Early containment in the epicenter and avoiding draconian social distancing
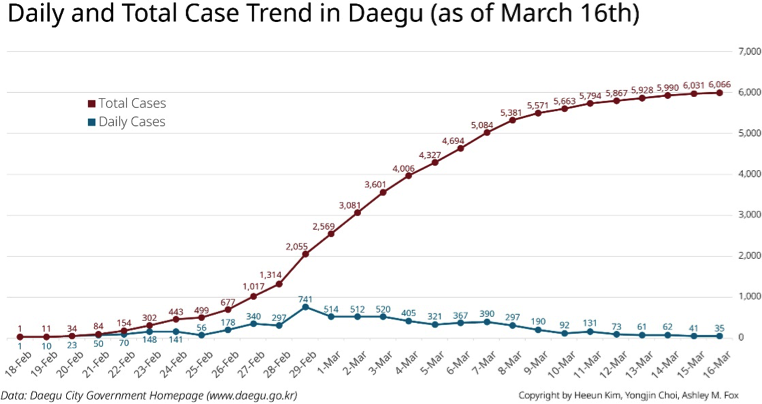
On Feb 24, the South Korean government announced that their response to COVID-19 would switch to a combination of containment and mitigation. Since the number of new cases in Daegu had been increasing at that time, they continued keeping the virus contained within Daegu and adjacent regions by testing about 37,000 people including members of Shincheonji Church of Jesus, a religious “cult” that is believed to be largely responsible for the spread of the virus initially, or citizens having fever or respiratory symptoms. The number of 37K people was based on an estimation using data on the number of flu patients in the Daegu area. The government aimed to detect and isolate as many cases as possible so that they could minimize the transmission within Daegu and neighboring areas.
Korea did not quarantine any part of the city of Daegu and did not use draconian social distancing either. They used national level, non-mandatory social distancing recommendations, except for the executive order on banning the services of Shincheonji. They strongly asked for voluntary social distancing including working at home and avoiding large gatherings. The only mandatory requirements were school and daycare center closures.
Thus, arguably, it seems that such an intensive containment strategy in the epicenter at an early stage contributed to turning the tide of new cases in South Korea. The graph shows the decrease in new cases in Daegu and South Korea as a whole after completing the exhaustive testing in Daegu. At the same time, the government is gradually switching to mitigation strategies that minimize the case fatality and community transmission in other regions.
- Importance of Rapidly Scaling-up Testing Capacity
Several weeks into community transmission, the US still does not have widespread testing available nor routine protocols in place to inform citizens on how to get tested. By contrast, South Korea has been testing over 10,000 people per day since March 1, though mass testing began earlier on Feb 21st in Daegu. Each county-level region has adopted an average of 2-3 testing sites where people with symptoms can get tested. The basic principle of testing is that anyone who is a suspected case is encouraged to get tested. Limiting the test to suspected case plays a role as a gatekeeper that prevents testing overloads. Similar to the current US testing protocol, if you have symptoms, you should call KCDC Call Center or primary care doctor first. They will ask you a series of questions and if you meet certain criteria, you are deemed a suspected case, and you might be recommended you go get tested at certain testing sites.
Boosting physical accessibility. One innovation that is credited with having rapidly scaled up testing in Korea is the availability of “drive-thru” testing stations to carry heavy caseloads efficiently. In drive-through testing sites, patients can stay in their cars and be swabbed for the virus. Drive-through testing has been reported to have the capacity to test six people per hour, whereas regular testing places test two people per hour. Further, there is a low risk of cross-infection since the drivers are tested inside their car, and testing places do not need negative pressure rooms as well. It has been a vital part of the rapid expansion of testing in Korea.
Physical and financial accessibility. While much attention has been given to drive-thru testing centers in Korea,in addition, testing centers located in community health centers and tertiary hospitals in the region, which were well-known to residents, were made easily accessible for testing. Private hospitals that had existing negative pressure rooms and isolation wards were designated as official testing sites and supported to carryout testing by the government. On the other hand, there were some early criticisms that the government “forced” these clinics and hospitals to run test sites without any discussions beforehand.
National health insurance reduced transaction costs. Testing and treatment in the US has been hampered by a lack of universal health coverage raising questions about whether citizens will avoid testing and put off necessary care to avoid medical bills. In contrast with President Trump’s statements in his address to the nation, US insurance companies have only committed to waiving co-pays and fees for people with insurance to be tested for COVID-19, but not for any of the care that uninsured Americans (presently 28 million people) might require if they are hospitalized. By contrast, in Korea, the government quickly committed to pay for all expenditures related to testing and treatment of COVID-19 patients by having the National Health Insurance cover all hospital bills. National Health Insurance covers not only the testing itself but also everything in treatment.
Avoiding unnecessary testing and rationalizing the response. While increasing testing capacity has been a key piece of the response, in order to avoid overwhelming the country’s testing capacity, Korea also built in disincentives to avoid unnecessary testing. If you get tested without being a suspected case or without a doctors’ referral, and end up testing negative, you will need to pay $150 for the test out-of-pocket. If you undergo chest x-rays and computed tomography (CT) under these same conditions, the total cost will be around $200. This is a steep cost for most Koreans. There is some evidence that this policy has deterred some unnecessary (or unindicated) testing as many people go back to their homes when they realize this policy at testing sites. This policy plays a gatekeeper role that has prevented the overloading of testing sites and ensured the targeting higher-risk groups first. On the hand, it could discourage people with more mild symptoms from testing, masking broader infection levels.
- Responses to overwhelmed health systems and resources
Beds and staff
As countries like Italy are already in a situation where they are facing the need to triage patients due to an overwhelming of their healthcare system, it is worthwhile to reflect on how Korea has been able to keep up with increased demand for intensive care. Although South Korea has 12.27 hospital beds per 1,000 people (as of 2017), which is relatively high compared with OECD countries (US had 2.77 beds per 1,000 in 2016), the explosion of COVID-19 cases overwhelmed the healthcare system. At the same time, people with chronic diseases were reluctant to visit hospitals for their regular checkup, which has proven costly in some cases. For example, one case of hospital-level cluster transmission in Seoul was triggered by a chronic disease patient from the city of Daegu. She was unable to get an appointment with a doctor in several clinics and hospitals in Seoul after revealing she was from Daegu, which resulted in her hiding the fact that she was from Daegu from another hospital. She ultimately tested positive for COVID-19 and the hospital was forced to close for a time, which posed a heavy burden for the hospital and its staff.
One approach the government took to manage the overwhelming of its resources was to classify COVID-19 patients into several layers and treat them in different places, known as “trace, test and treat.” Patients in severe condition are being treated in tertiary hospitals, whereas patients with mild cases are treated in residential centers. Further, the government asked hospitals to isolate patients with respiratory symptoms from patients with non-respiratory symptoms, so that people with other chronic conditions can visit hospitals for meeting with doctors. These measures appear to have been effective in limiting the amount of triaging required. However, the city of Daegu, the epicenter of Korea’s outbreak, did in fact experience a shortage of beds and staff as the number of patients soared. Lack of beds in some cases led to higher case fatality as several patients died at home while waiting for a bed for treatment.
Face Masks
While the question of whether wearing a face mask is effective in preventing the spread of the virus is a source of controversy, wider cultural acceptance of face masks in Korea may be playing a role in containment. While the US Center for Disease Control and Prevention recommended people not to wear face masks unless they are in close contact with someone infected or infected themselves, many Asian countries encourage people to wear them. In South Korea, wearing face masks was officially encouraged as one of the most important sources of personal protection, thereby causing a shortage of facial masks across the country. People started to hoard face masks, and the price skyrocketed. Online deals for face masks were quickly sold out, which meant that some groups could not access them, especially marginalized populations with low digital literacy.
However, the Korean government quickly responded to the shortage of face masks by taking “full control” of the supply chain managing the entire process of production, logistics, and distribution of masks to distribute face masks fairly to all citizens. This included steps like limiting weekly sales of face masks for customers to two in local pharmacies and introducing odd-even rules– i.e., customers born on odd-numbered days can purchase masks on odd days and vice-versa. This rationing approach was enabled by pharmacies’ ability to check the customer’s mask purchasing record using the National Health Insurance database.
Despite much criticism about the program, i.e., long customer lines at pharmacies, confusing rules, and concerns about virus transmission in the waiting line, the government supplied 38 million face masks for the first week of this “public face masks” program. By contrast, the US has largely been relying on the voluntary acts of private businesses to enforce anti-price gouging and rationing measures.
It may take some time to see how successful these measures will be. However, so far, the South Korean case shows that the government can be an effective agent in managing resources during disease epidemics.
- Transparency in government
Regular communication from a “central control tower”. An additional facilitator of Korea’s response pertains to open communication channels, which facilitated trust and transparency. Amid the politicization and sensationalized media coverage of COVID-19, South Korea’s response to the epidemic has rested on maximizing its transparency. Since confirmed cases began spiking in February, a central control tower led by the prime minister, the director of the Korean Center for Disease Control (KCDC), and the minister of Department of Health and Human Service (DHHS) has been holding a regular press briefing twice a day. The number of tests, positive cases, persons under quarantine, and under investigation are reported in many ways, including through regular press briefings, reports, and press releases. Such multi-channel communication has maximized the transparency and accessibility of information, thereby keeping people updated on the rapidly evolving situation at least once a day.
One of the other communication channels is emergency text alerts sent from government agencies. Through the emergency text alerts, local governments can send text alerts to people when they have confirmed cases in their regions. This has helped people stay informed in real time about cases in their area and helped them make more informed decisions during the outbreak.
These updates have been facilitated by the availability of testing providing confidence in the accuracy of reported cases compared with, for instance, the US, where confirmed cases are believed to radically underrepresent true cases. Communication channels in the US are also complicated by the complex, decentralized federal, state and local channels of communication, which are not always well coordinated and the poor executive leadership exercised by President Trump.
However, there have been complaints that the emergency alerts are “too revealing” about patients’ private lives. Multiple alerts are being sent to people every day, telling the personal information about patients in their localities, which might be identifiable by neighborhoods. Further, people are turning off the alerts since they receive dozens of text messages from multiple government agencies, including “non-emergent” information. This raises a question of what is the right level of government transparency and amount of information to provide during an outbreak situation.
Facilitators of an Effective Response
Undergirding the government’s seemingly effective responses, social trust in the healthcare system, a coordinated response and effective policymaking appear to have served as facilitators of the Korean COVID-19 response to date, even in the absence of more draconian quarantine or social distancing measures that many Western democracies are now adopting. It may still be too early to know which aspects of the Korean response have been most effective and still too early to declare victory. However, a glimpse into the South Korean case gives us some lessons for the US government. Of course, South Korea is still one of the most impacted countries in the COVID-19 pandemic. However, it is noteworthy that expanding the accessibility of testing and transparent information plays a critical role in buffering the impacts of the outbreak. These are some of the
Joshua Busby is a Professor in the LBJ School of Public Affairs at the University of Texas-Austin. From 2021-2023, he served as a Senior Advisor for Climate at the U.S. Department of Defense. His most recent book is States and Nature: The Effects of Climate Change on Security (Cambridge, 2023). He is also the author of Moral Movements and Foreign Policy (Cambridge, 2010) and the co-author, with Ethan Kapstein, of AIDS Drugs for All: Social Movements and Market Transformations (Cambridge, 2013). His main research interests include transnational advocacy and social movements, international security and climate change, global public health and HIV/ AIDS, energy and environmental policy, and U.S. foreign policy.


0 Comments