This is a guest post from Hina Khalid and Ashley Fox. Hina Khalid, PhD, MPP is an Assistant Professor in the School of Humanities and Social Sciences, Information Technology University, Lahore, Pakistan. Her work focusses on health policy with a special interest in health system performance and health inequities. She can be found on Twitter @HinaaaKh. Ashley Fox, PhD, MA, is an Assistant Professor of Public Administration and Policy at Rockefeller College of Public Affairs and Policy, University at Albany, SUNY, who researches the politics of health policy and population health. She can be found on Twitter @ashfoxly.
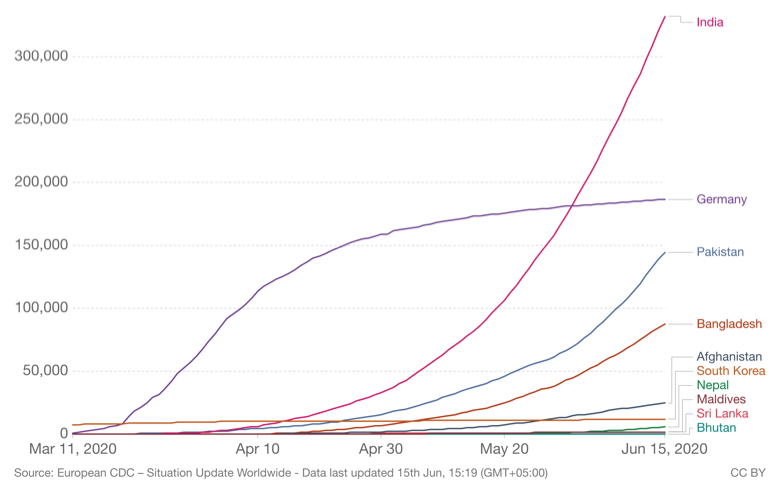
As the global COVID-19 pandemic soars to 4.1 million cases, the search to identify the ingredients of a “successful” national response has already begun in earnest. This yearning to categorize and make predictions forces us to assess our priors about what characteristics of states might be likely to produce better or worse than anticipated outcomes. This includes revisiting classical debates around whether more centralized “command and control” states may be better at epidemic control versus more decentralized, flexible forms of governance.
So far, the countries with the seemingly most “successful” responses that have kept the virus contained appear to be more centralized regimes including a number of East Asian countries, Iceland and New Zealand. Certainly, in the case of the US, the decentralized federal structure does not appear to be acting as an asset in this pandemic. The differential timing of lockdowns and re-opening of the economy will undoubtedly allow the virus to continue to spread even when it has been contained in one locale, especially with the failure to bring testing to scale. Rather than acting as a unified force, states are being made to compete against each other for emergency resources.
Finding appropriate responses, given resource constraints, is especially important in low- and middle-income countries like Pakistan, which are often described as weak or lacking capacity. Pakistan instituted devolution in 2011, including devolving health policy formation, coordination, and implementation to the country’s four provinces. In this post we examine Pakistan’s response to COVID-19 to date, placing it in the perspective of past infectious disease responses and use this to re-examine the question of whether decentralization strengthens or weakens states’ ability to respond to infectious disease threats.
The cases of countries that successfully battled COVID are also relatively small and homogenous states that arguably share characteristics other than being centralized that predispose them to a more effective response. Further, Germany, a federal state has served as a model for other high-income countries for its methodical response suggesting that decentralized states can effectively coordinate across units to mount effective responses to communicable disease.
While centralized states have historically been considered to be better able to formulate policy independent of social groups and to carry out policy without obtrusion, decentralization has been advocated for several decades for states with weak national institutions and political tensions caused by ethnic, religious, ideological or other cleavages. Centralized states may be strong in some respects, but they can also be “brittle” in others. They may feed tensions among fractious groups, leading to violence. They may be unresponsive, inefficient, or wasteful in the use of public resources. And they may facilitate a tyranny of the majority or elite state capture on a national scale.
In Pakistan, decentralization has both helped and hampered the response. On the one hand, it has enabled the provinces to take ownership of their responses and demonstrate innovation, while on the other it has increased the complexity around coordinating policy responses. However, over and above decentralization, the country’s response has been constrained by low public health capacity, politics, and inadequate governance.
Features of Pakistan’s response to COVID-19
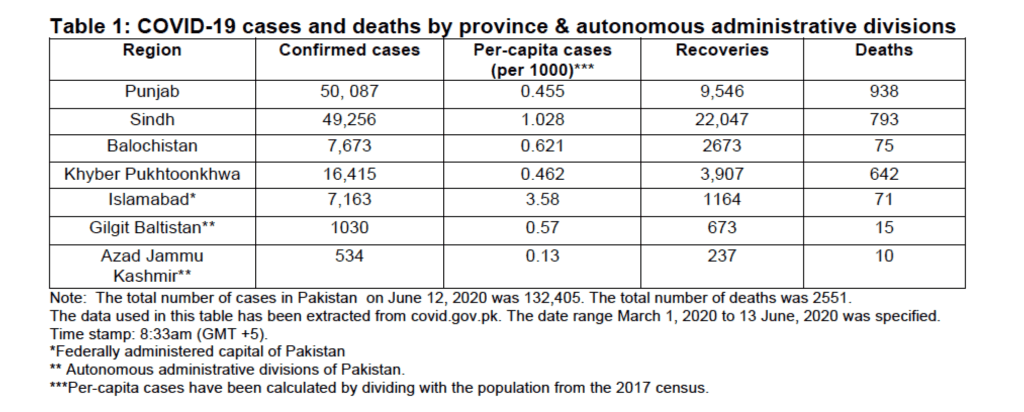
The number of COVID-19 cases has been rapidly increasing across Pakistan’s four provinces (Punjab, Sindh, Khyber Pukhtoonkhwa (KPK) and Balochistan) and federally administered territories since March 2020. Broadly, the country’s response has focused on implementing a lockdown which has been reassessed several times and more recently, has been eased drastically; testing, contact tracing and quarantining citizens; and a relief package by the center, the Ehsaas Emergency Program.
The center has been coordinating the response at the national level, filling in gaps in service provision and providing emergency income assistance to citizens below the poverty line through the Ehsaas Emergency Program. COVID-19 related planning, coordination, and implementation is being achieved through two newly established committees, the National Coordination Committee (NCC) and the National Command and Operation Centre (NCOC), which have been formed keeping in view the absence of coordination mechanisms between the center and provinces. While the first two cases of coronavirus in Pakistan were confirmed at the end of February, as late as mid-March, the center remained reluctant to impose a lockdown, and asked citizens to self-quarantine.
In a national televised address, the Prime Minister, expressed concern that while implementing a lockdown would curb the spread of the virus, it could also lead to deaths from poverty. Consequently, before the center could reach a decision and in light of the increasing number of coronavirus cases, the provinces went ahead and implemented lockdowns, with the province of Sindh leading the way. More recently, the center and provinces have gradually been easing the lockdowns.
The provinces have had the leeway to experiment with different strategies related to testing, implementation of lockdowns and their easing, and expansion of financial laboratory for innovation, provinces have varied in their approaches, which has the potential to generate innovative solutions. They have experimented with different types of testing strategies, relief packages, and have varied the speed and mix of how lockdowns are being eased. However, responses are being constrained by low public health capacity.
The provinces have also differed in how responsive they have been to pressures from religious communities to re-open mosques reflecting the power of religious groups in those regions. These differences across provincial responses reflect the underlying political and social make-up of the provinces. Consequently, inter-province competition, pressure from interest groups and low-state capacity/legitimacy has the potential to threaten the positive aspects of decentralized governance systems in the response to COVID-19.
Devolution and COVID-19 in Pakistan
Pakistan has frequently been categorized as a weak state due to its low-capacity civil institutions, frequent ethnic disputes, and the power of the military vis-à-vis civilian regimes (see Council on Foreign Relations). Under political pressure, the 18th Amendment, adopted in 2011, instituted devolution aimed at rolling back decades of infringements on Pakistan’s constitution by military rulers. It aimed to restore democracy to its original form and reduce the powers that had been vested in presidents at the expense of the parliamentary form of government.
Administratively, devolution is an advanced form of decentralization as it involves divesture of responsibility at the center. Following devolution, the Ministry of Health was dissolved though later reconstituted as the Ministry of National Health Services, Regulation and Coordination and health policy formation, coordination, and implementation, was devolved to the provinces.
The four provinces are ethno-linguistically diverse and also vary in terms of poverty levels. In terms of ethnic domination, the Urdu-speaking migrant elite (Muhajirs) and Punjabis have exercised higher levels of control over the state apparatus and have driven perceptions of exclusion and marginalization among the smaller ethnic groups. In addition to linguistic diversity, the religious and sectarian make-up of Pakistan has also been a cause of conflict in recent years.
Multi-dimensional poverty (deprivation levels based on lack of access to education, health, housing, and an unsafe living environment) is lowest in Punjab and highest in Balochistan. KPK and Sindh lie in the middle with no significant difference in their multi-dimensional poverty levels. While in theory, decentralization can enable diverse jurisdictions to respond more effectively to an infectious disease outbreak in a variety of ways, in practice, the results are mixed.
Decentralization has enabled the provinces to implement local solutions and has provided them with an opportunity to act as “laboratories of innovation.” To offset the economic impacts of the lock down, the national government implemented a cash assistance national Ehsaas Emergency Program, which several provinces have emulated, introducing additional relief packages to ease financial hardship faced by households. For example, KPK announced a relief package of Rs. 11.4 billion, and Punjab a package of Rs. 10 billion alongside a waiver of Rs. 18 billion in taxes. The provinces have deployed a range of measures to increase their testing and public health capacities and a sense of competition to outperform other jurisdictions is evident.
These measures have involved engaging with the center (National Institute of Health and National Disaster Management Authority) and the private sector. Some examples of the use of the private sector include the increased use of private labs for testing, drive through testing facilities, development of human resources, tele ICU consultation services, and varied forms of testing and surveillance. They are also employing different types of testing strategies. Punjab is employing a smart sampling approach (i.e. collecting and testing samples from randomly selected households) while KPK will be prioritizing testing of healthcare workers and contacts of COVID-19 patients. The province has also announced that community-based surveillance (i.e. testing people in the vicinity of a coronavirus case, but without contact history) will be carried out if deemed necessary. Balochistan is only testing a limited number of people due to extreme lack of testing capacity.
Variation has been observed in how the lockdown is being eased. Across provinces, some examples include, easing restrictions on businesses, mosques, public transport, and opening shopping centers. Following an easing of restrictions on select businesses, mosques were opened for congregational prayers during the month of Ramadan across all provinces with the exception of Sindh. Restrictions on public transport have recently been lifted in KPK, Punjab, and Sindh. In terms of shopping malls, the province of Punjab has allowed malls to open with minor restrictions, while in Sindh children and people above the age of 55 are not allowed to enter shopping malls. In KPK, markets are open with limited hours. However, across all provinces, violations of social distancing guidelines has led to shops and markets being sealed. (See table 2)
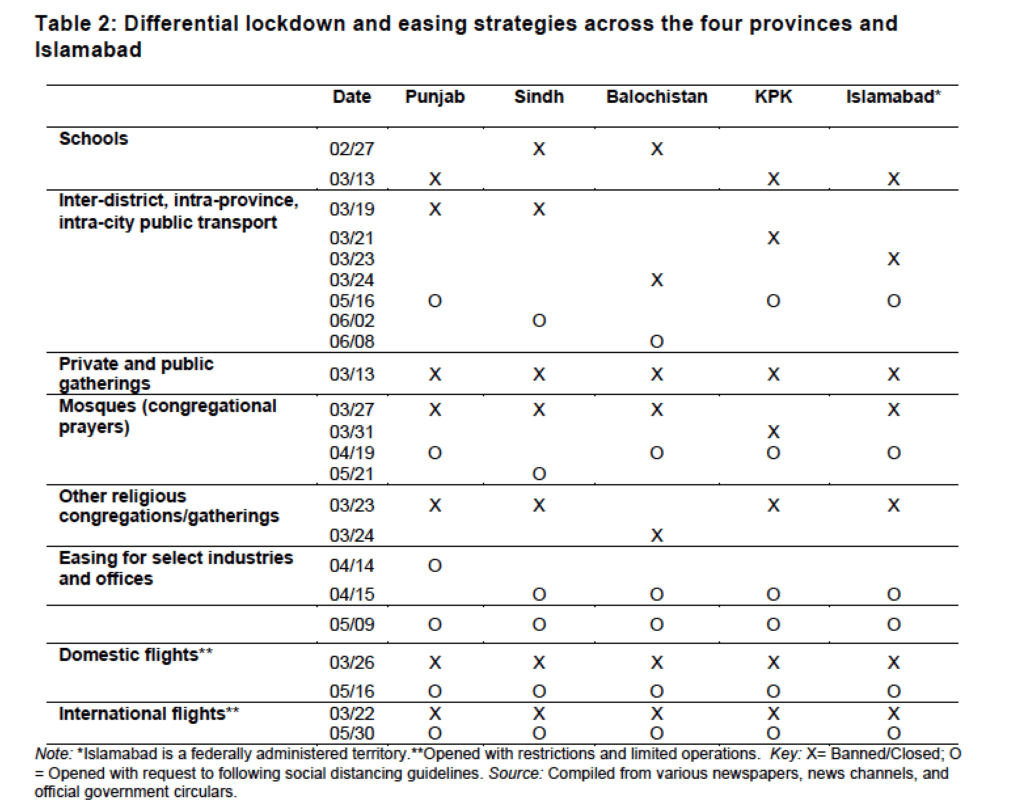
Other aspects of the response have included initiatives to support health workers. For example, Punjab is providing healthcare workers with bonuses and insurance, while KPK has introduced a special package to provide financial support for families of health care workers who lose their lives while handling patients. Sindh is also set to introduce a package along similar lines. Various measures have also been announced to facilitate businesses. Thus, devolution has enabled experimentation with diverse policy approaches that have the potential to be more or less effective at bending the curve while reducing the financial hardship stemming from the lockdowns.
However, low public health capacity and inadequate governance is constraining the response. The capacity and governance constraints being experienced today, pre-date devolution and while devolution aimed to address these issues (in addition to increasing provincial autonomy) they continue to persist. Devolution of health in Pakistan was imposed in an ad-hoc and abrupt manner.
During the course of in-depth interviews with HIV program employees and health experts from donor organizations in 2015 we learnt that the provinces had to perform expanded functions for which they did not have the capacity and expertise as they did not have the opportunity to build capacity prior to the move, in their words “we were shell shocked”.
Following devolution, health expenditures have increased, yet continue to remain low. Low public health capacity, an unbalanced distribution of doctors, a reduction in the focus on health promotion and prevention, and inequities in quality, access, and availability of health services continue to undermine provision of health services. Moreover, clustering of technical assistance reforms in better performing provinces has, possibly, exacerbated inequities across the provinces. It is not surprising then, that some provinces face more severe capacity issues as compared to others which has hampered both testing as well as the safety of the medical community.
Citizen confidence in the health system has remained low and low compliance by citizens could plausibly be the outcome of low-overall confidence in the health system, low trust in government or unclear and inconsistent public health messaging since the pandemic started. More recently, despite the sharp surge in cases, the Supreme Court, added to the confusion by issuing a “suo-motu” notice which details that corona virus is “not a pandemic in Pakistan” and large shopping malls to be re-opened. Appeals to seek the advice of medical experts on this matter were ignored by the Supreme Court.
Decentralization has provided the central government an opportunity to focus on the overarching aspects of the response (macro versus micro-level details), possibly freeing up space for ensuring a more coordinated response at the national level. However, it has also placed increasing demands for coordination both within and across government tiers which has proven to be complex. Vertical coordination has been challenging. The center had a delayed response around the features of an appropriate lockdown strategy, which nudged the provinces into introducing lockdowns ahead of the center.
Moreover, perception of delayed and inadequate screening procedures at airports by the center further strained the relationship between the center and the provinces. Especially for Pakistan, coming out of devolution, the center and provinces had unresolved resource and administrative issues which strained the relationship over the past decade, and little progress has been made in terms of establishing a regular dialogue across the government tiers. The regulatory capabilities of the federal ministry also remain questionable. The establishment of the NCC and the NCOC in the on-going pandemic is a positive step as it is an effort to connect the center and provincial governments to ensure a multi-sectoral response.
In terms of horizontal coordination, varying levels of governance and public health capacities across the provinces has hampered effective coordination thereby increasing the threat of spill-over effects from one jurisdiction to another. Apart from varying speeds of lockdown, where the province of Sindh was the first to respond, the provinces of Punjab and Balochistan, arguably took delayed and ineffective action in terms of suspending a religious Tableeghi-Jamaat congregation, and screening religious pilgrims from the Taftaan border respectively. The country has paid a heavy price in terms of a high number of COVID-19 cases for both these instances of mismanagement. However, the government continues to cave in to pressure from religious clerics. The federal government reopened mosques in the month of Ramadan in spite of strong advice to the contrary by the medical community, a move adopted by all provinces except the province of Sindh. This response is not surprising as religious clerics form a strong interest group in Pakistan, and have been gaining power over the past few decades. In the past, they have hampered the effectiveness of health interventions around contentious issues such as HIV/AIDS and the government has often resorted to indirect means to achieve its public health goals in these domains to avoid confrontation.
Towards building a strong state
Evidence coming out of Pakistan is mixed in terms of the relationship between decentralization and a state’s ability to respond to a pandemic. On the one hand, decentralization has enabled the subnational units to display ownership and take initiative in building their public health capacities. On the other hand, coordination challenges have been observed across the center and provinces. Over and above devolution, however, it is apparent that the response has been constrained by low public health capacity, politics, and inadequate governance.
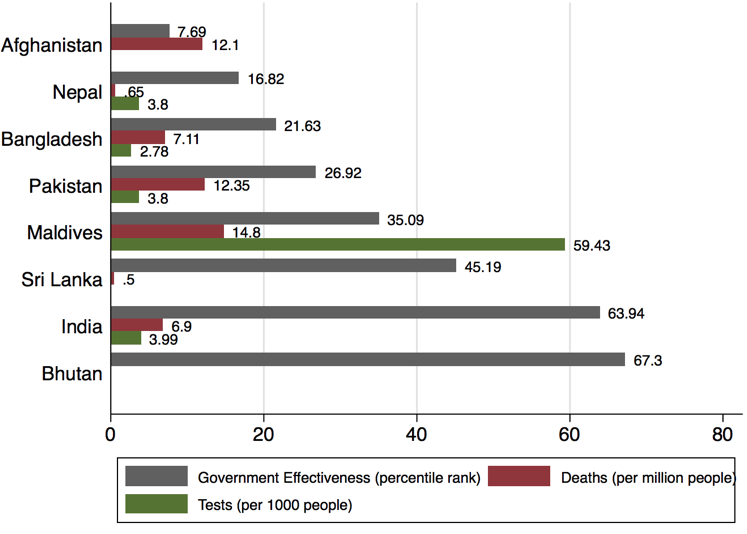
Source: Worldwide Governance indicators, Our World in Data, deaths & tests. Note: (1) Government effectiveness is given on a scale of 0-100 (lowest to highest) and reflects data for 2018. (2) Data for deaths reflects the aggregate values for June 15,2020. Data for Bhutan reflected 0. (3) Data for tests reflects the following: June 13 - India & Pakistan, June 11 – Bangladesh, June 10 –Nepal & Maldives. Data for Afghanistan, Sri Lanka and Bhutan was not available.
Pakistan’s performance on the governance indicator, government effectiveness, for 2018 has remained low in comparison to the overall average for South Asia (35.58) and several South Asian countries (India, Maldives, Sri Lanka and Bhutan). Government effectiveness captures perceptions of quality of public and civil services, the degree of independence from political pressures, and the quality of policy formation as well as credibility and implementation. (See Figure 2) These numbers suggest a need for enhancing government performance, especially when viewed alongside COVID-19 related deaths and testing capacity (as reflected by tests per 1000 people) in the country.
These challenges highlight the need and importance of focusing attention towards building a stronger state capacity, which does not necessarily have to mean a centralized state. According to Price-Smith, Tauber & Bhat (2004), “the foremost explanation as to why some states adapt more effectively [to disease outbreaks] than others is based on the notion of state capacity, which reflects the endogenous resources that a state may mobilize in order to deal with emergencies, such as epidemic disease.” Whereas classical definitions conceive of strong states as centralized (i.e., unitary rather than federal) where power is concentrated in the executive branch, in a pandemic, if the central government response is lackluster, this can at least partially be mitigated by more effective responses from sub-units and policy learning can be transferred from sub-national units to the federal level.
Other conceptualizations of weak states, describe them as states that are “unable to formulate policy goals independent of particular groups in society” (Vogel, 1986). In Pakistan, religious clerics have, yet again, emerged as a powerful interest group which has undermined the response. Additionally, statements by the judiciary, one of the most essential arms of the state, such as that coronavirus is “not a pandemic in Pakistan” threaten to undermine containment efforts by different government tiers. The lack of compliance by citizens also suggests a need to revisit the state-citizen relationship and factors that have shaped it over the past few decades.
The pandemic has highlighted that greater work is required in terms of enhancing the resource capacity, coordinative capacity, and coercive capacity of the state, as well as its reach. Going forward attention can be focused on enhancing state strength and enabling different tiers of government to perform functions they are best placed to perform.
Joshua Busby is a Professor in the LBJ School of Public Affairs at the University of Texas-Austin. From 2021-2023, he served as a Senior Advisor for Climate at the U.S. Department of Defense. His most recent book is States and Nature: The Effects of Climate Change on Security (Cambridge, 2023). He is also the author of Moral Movements and Foreign Policy (Cambridge, 2010) and the co-author, with Ethan Kapstein, of AIDS Drugs for All: Social Movements and Market Transformations (Cambridge, 2013). His main research interests include transnational advocacy and social movements, international security and climate change, global public health and HIV/ AIDS, energy and environmental policy, and U.S. foreign policy.


0 Comments